Ati
| Ati | |
|---|---|
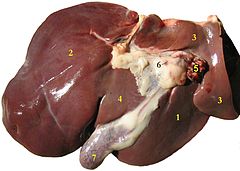 Ati wedhus: (1) lobus tengen, (2) lobus kiwa, (3) lobus mawa buntut, (4) lobus kuadratus, (5) arteri ati lan vena portal, (6) klanjer getah bening ati, (7) kanthong empedu. | |
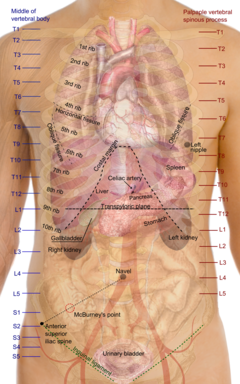 Proyeksi lumahing organ torso, nuduhaké ati ing tengah | |
| Rincian | |
| Purwaka | foregut |
| Vena | vena hepatika, portal vena hepatika |
| Saraf | celiac ganglia, vagus[1] |
| Pengenal | |
| Latin | jecur, iecer |
| MeSH | D008099 |
| TA98 | Masalah skrip: Fungsi "getTAValue" ora ana. |
| TA2 | 3023 |
| FMA | 7197 |
| Terminologi anatomi [[[d:Masalah skrip: Fungsi "pageId" ora ana.|besut ing Wikidata]]] | |

Ati (Grikenlan: ἡπαρ, hēpar) wujud klanjer gedhé dhéwé ing njero awak, manggon ana njero gronggongan weteng sisih tengen, peneré ing sangisoré diafragma. Ati iku sawijining organ ing vèrtebrata, kalebu manungsa. Organ iki duwé peran wigati ing métabolisme lan duwé sapérangan fungsi ing awak/badan kalebu panyimpenan glikogen, sintesis protéin plasma, lan netralaké obat. Ati uga mrodhuksi bile, kang wigati kanggo pancernan.
Adhedhasar fungsiné, ati uga kalebu minangka piranti èkskrèsi. Iki amarga ati mbiyantu fungsi ginjel kanthi cara mecah sapérangan senyawa kang asifat racun lan ngasilaké amonia, urea, lan asem urat kanthi mupangataké nitrogen saka asem amino. Prosès pamecahan senyawa racun déning ati diarani prosès detoksifikasi.
Lobus ati kawangun saka sèl parenkimal lan sèl non-parenkimal.[2] Sèl parenkimal ing ati diarani hepatosit, manggoni watara 80% volume ati lan nglakokaké manéka fungsi utama ati. 40% sèl ati ana ing lobus sinusoidal. Hepatosit wujud sèl endodermal kang kastimulasi déning jaringan mesenkimal kanthi terus-terusan wiwit embrio nganti ngrembaka dadi sèl parenkimal.[3] Sakwéné wektu mau, dumadi paningkatan transkripsi mRNA albumin minangka stimulan proliferasi lan diferensiasi sèl endodermal dadi hepatosit.[4]
Lumen lobus kawangun saka SEC lan dipanggoni déning 3 jinis sèl liya, kaya ta sèl Kupffer, sèl Ito, limfosit intrahepatik kaya ta sèl pit. Sèl non-parenkimal manggoni watara 6,5% volume ati lan mrodhuksi manéka substansi kang ngendhalèkaké akèh fungsi hepatosit.
Filtrasi wujud salah siji fungsi lumen lobus sinusoidal kang misahaké lumahing hepatosit saka getih, SEC duwé kapasitas endositosis kang gedhé banget kanthi manéka ligan kaya ta glikoprotein, komplèks imun, transferin lan seruloplasmin. SEC uga duwé fungsi minangka sèl presenter antigen kang nyedhiakaké èksprèsi MHC I lan MHC II kanggo sèl T. Sèkrèsi kang dumadi ngambah manéka sitokina, eikosanoid kaya ta prostanoid lan leukotriena, endotelin-1, nitrogen monoksida lan sapérangan komponèn ECM.
Sèl Ito ana ing jaringan perisinusoidal, wujud sèl kanthi akèh vesikel lemak ing njero sitoplasma kang ngiket SEC kuwat banget nganti mènèhaké lapisan gandha ing lumen lobus sinusoidal. Nalika ati ana ing kaanan normal, sèl Ito nyimpen vitamin A guna ngendhalèkaké kalenturan matriks èkstraselular kang diwangun mawa SEC, kang uga wujud kalenturan saka lumen sinusoid.
Sèl Kupffer ana ing jaringan intrasinusoidal, wujud makrofaga kanthi kamampuan endositik lan fagositik kang ngéramaké. Sèl Kupffer sadina-dina interaksi karo matérial kang asalé saka saluran pancernan kang ngandhut larutan bakterial, lan nyegah aktivasi èfèk toksin senyawa mau menyang njero ati. Paparan larutan bakterial kang dhuwur, mligi paparan LPS, gawé sèl Kupffer nglakokaké sèkrèsi manéka sitokina kang micu prosès paradhangan lan bisa ngakibataké tatu ing ati. Sèkrèsi antarané ngambah spesi oksigèn reaktif, eikosanoid, nitrogen monoksida, karbon monoksida, TNF-α, IL-10, minangka rèspon kakebalan turunan sajeroning fasa infèksi primèr.
Sèl pit wujud limfosit kanthi granula gedhé, kaya sèl NK kang manggon ing ati. Sèl pit bisa ngindhuksi pepati sanalika ing sèl tumor tanpa gumantung ing èksprèsi antigen ing komplèks histokompatibilitas utama. Aktivitas sèl pit bisa ditingkataké kanthi stimulasi interferon-γ.
Saliyané iku, ing ati isih ana sèl T-γδ, sèl T-αβ lan sèl NKT.
Sebutan medhis kang ana gandhéngané karo ati lumrahé diwiwiti nganggo hepat- utawa hepatik saka tembung Yunani kanggo ati, ya iku hepar.
Sèl punca[besut | besut sumber]
Saliyané hepatosit lan sèl non-parenkimal, ing ati isih ana jinis sèl liya ya iku sèl intra-hepatik kang asring diarani sèl oval,[5] dan hepatosit duktular.[6] Régénerasi ati sawisé hepatektomi parsial, lumrahé ora nglibataké sèl progenitor intra-hepatik lan sèl punca èkstra-hepatik (hemopoietik), lan gumantung mung marang proliferasi hepatosit. Nanging sajeroning kaanan nalika proliferasi hepatosit kacandhet utawa katundha, sèl oval kang ana ing aréa periportal bakal ngalami proliferasi lan diferènsiasi dadi hepatosit diwasa.[5][7] Sèl oval wujud wangun diferènsiasi saka sèl progenitor kang ana ing aréa portal lan periportal, utawa kanal Hering,[8] lan mung tinemu nalika ati ngalami cidra.[9] Proliferasi kang dumadi ing sèl oval bakal minangka saluran èkskrèsi kang ngubungaké aréa parenkima papan dumadiné karusakan ati karo saluran empedu. Epimorfin, sawijining morfogen kang akèh tinemu duwé peran ing akèh organ epitelial, katoné uga duwé peran ing pambentukan saluran empedu déning sèl punca hepatik.[10] Sawisé iku sèl oval bakal kadiferensiasi dadi hepatosit duktular. Hepatosit duktular dianggep wujud sèl transisi kang magepokan antarané karo:[11]
- metaplasia duktular saka hepatosit parenkimal dadi epitelium biliari intra-hepatik
- konvèrsi metaplasia saka epitelium duktular dadi hepatosit parenkimal
- diferensiasi saka sèl punca saka silsilah hepatosit
gumantung ing jinis gangguan kang nyerang ati.
Ing modhèl tikus kanthi 70% hepatektomi, lan indhuksi regenerasi hepatik kanthi asetilaminofluorena-2, tinemu yèn sèl punca kang asalé saka sungsum balung mburi bisa kadiferensiasi dadi hepatosit,[12][13] kanthi médhiasi hormon G-CSF minangka kemokina lan mitogen.[14] Regenerasi juga dapat dipicu dengan D-galaktosamina.[15]
Sèl imunologis[besut | besut sumber]
Ati uga duwé peran sajeroning sistem kakebalan kanthi akèhé sèl imunologis ing sistem retikuendotelial kang duwé fungsi minangka tapis antigen kang kagawa menyang ati liwat sistem portal ati. Papindhahan fasa infèksi saka fasa primèr dadi fasa akut, ditengeri déning ati kanthi ngedhunaké sekresi albumin lan ngunggahaké sekresi fibrinogen. Fasa akut kang terus-terusan bakal ngakibataké simtoma hipoalbuminemia lan hiperfibrinogenemia.[16]
Nalika ati cidra, sèl getih putih bakal distimulasi kanggo migrasi nuju ati lan bebarengan karo sèl Kupffer nyekresi sitokina kang gawé modhulasi prilaku sèl Ito.[17] Sèl TH1 mrodhuksi sitokina kang ngundhakaké rèspon kakebalan selular kaya ta IFN-gamma, TNF, lan IL-2. Sèl TH2 suwaliké bakal mrodhuksi sitokina kang ngundhakaké rèspon kakebalan humoral kaya ta IL-4, IL-5, IL-6, IL-13 lan ngundhakaké rèspon fibrosis. Sitokina kang disekresi déning sèl TH1 bakal nyandhet diferensiasi sèl T dadi sèl TH2, suwaliké sitokina sekresi TH2 bakal nyandhet proliferasi sèl TH1. Mula rèspon kakebalan asring ditélakaké kapolarisasi menyang rèspon kakebalan selular utawa humoral, nanging durung tau kaloroné.
Fungsi ati[besut | besut sumber]
Manéka jinis tugas kang dilakokaké déning ati, dilakokaké déning hepatosit. Nganti saiki durung tinemu organ liya utawa organ gawéan utawa piranti kang bisa nggantèkaké kabèh fungsi ati. Sapérangan fungsi ati bisa digantèkaké kanthi prosès dialisis ati, nanging tèknologi iki isih terus dikembangaké kanggo perawatan panandhang gagal ati.
Minangka klanjer, ati ngasilaké:
- empedu kang nganti ½ liter saben dina. Empedu wujud cuwèran semu ijo lan rasané pait, asalé saka hemoglobin sèl getih abang kang wis tuwa, kang banjur disimpen ing njero kanthong empedu utawa dièkskrèsi menyang duodenum. Empedu ngandhut kolesterol, garam mineral, garam empedu, pigmèn bilirubin, lan biliverdin. Sekresi empedu migunani kanggo nyerna lemak, ngaktifaké lipase, mbiyantu daya absorpsi lemak ing usus, lan ngowahi dat kang ora larut sajeroning banyu dadi dat kang larut sajeroning banyu. Yèn saluran empedu ing ati kabumpet, empedu lumebu menyang parédharan getih saéngga kulit panandhang dadi semu kuning. Wong kang mangkono iku diarani nandhang lelara kuning.
- sapérangan gedhé asem amino
- faktor koagulasi I, II, V, VII, IX, X, XI
- protéin C, protéin S lan anti-trombin
- kalsidiol
- trigliserida liwat lintasan lipogenesis
- kolesterol
- insulin-like growth factor 1 (IGF-1), sawijining protéin polipeptida kang duwé peran wigati sajeroning pertumbuhan awak ing sajeroning mangsa bocah lan tetep duwé èfèk anabolik ing wong diwasa.
- enzim arginase kang ngowahi arginina dadi ornitina lan urea. Ornitina kang dumadi bisa ngiket NH³ lan CO² kang asifat racun.
- trombopoietin, sawijining hormon glikoprotein kang ngendhalèkaké prodhuksi keping getih déning sungsum balung mburi.
- Ing triwulan awal pertumbuhan janin, ati wujud organ utama sintesis sèl getih abang, nganti tekan sakiwa-tengené sungsum balung mburi bisa njupuk alih tugas iki.
- albumin, komponèn osmolar utama ing plasma getih.
- angiotensinogen, sawijining hormon kang duwé peran kanggo ngundhakaké tekanan getih nalika diaktivasi déning renin, sawijining enzim kang disekresi déning ginjel nalika dikawruhi kurangé tekanan getih déning juxtaglomerular apparatus.
- enzim glutamat-oksaloasetat transferase, glutamat-piruvat transferase lan laktat dehidrogenase
Saliyané nglakokaké prosès glikolisis lan siklus asem sitrat kaya sèl ing lumrahé, ati uga duwé peran sajeroning metabolisme karbohidrat liyané:
- Glukoneogenesis, sintesis glukosa saka sapérangan substrat asem amino, asem laktat, asem lemak non ester lan gliserol. Ing manungsa lan sapérangan jinis mamalia, prosès iki ora bisa ngonvèrsi gliserol dadi glukosa. Lintasan ditambah rikat déning hormon insulin sairing karo hormon tri-iodotironina liwat patambahan laju siklus Cori.[18]
- Glikogenolisis, lintasan katabolisme glikogen dadi glukosa kanggo dieculaké menyang getih minangka rèspon ningkaté kabutuhan ènèrgi déning awak. Hormon glukagon wujud stimulator utama keloro lintasan glikogenolisis lan glukoneogenesis nglirwakaké awak saka simtoma hipoglisemia. Ing modhèl tikus, defisiensi glukagon bakal nyandhet kaloro lintasan iki, nanging ngundhakaké toléransi glukosa.[19] Lintasan ini, bersama dengan lintasan glukoneogenesis padha saluran pencernaan dikendalikan olèh klanjer hipotalamus.[20]
- Glikogenesis, lintasan anabolisme glikogen saka glukosa.
lan ing lintasan katabolisme:
- degradasi sèl getih abang. Hemoglobin kang kakandhut ing njeroné dipecah dadi dat wesi, globin, lan heme. Dat wesi lan globin didhaur ulang, éwadéné heme dirombak dadi metabolit kanggo dièkskrèsi bebarengan empedu minangka bilirubin lan biliverdin kang warnané ijo semu biru. Ing njero usus, dat empedu iki ngalami oksidasi dadi urobilin saéngga warna feses lan urin semu kuning.
- degradasi insulin lan sapérangan hormon liya.
- degradasi amonia dadi urea
- degradasi dat toksin kanthi lintasan detoksifikasi, kaya metilasi.
Ati uga nyadhangaké sapérangan substansi, saliyané glikogen:
- vitamin A (cadhangan 1–2 taun)
- vitamin D (cadhangan 1–4 sasi)
- vitamin B12 (cadhangan 1-3 taun)
- dat wesi
- dat tembaga.
Régénerasi sèl ati[besut | besut sumber]
Kamampuan ati kanggo nglakokaké régénerasi wujud sawijining prosès kang wigati banget supaya ati bisa pulih saka karusakan kang ditimbulaké saka prosès detoksifikasi lan imunologis. Régénerasi kagayuh kanthi interaksi kang komplèks banget antara sèl kang ana sajeroning ati, ing antarané hepatosit, sèl Kupffer, sèl endotelial sinusoidal, sèl Ito lan sèl punca; karo organ ekstra-hepatik, kaya ta klanjer tiroid, klanjer adrenal, pankreas, duodenum, hipotalamus.[21]
Hépatosit, iku sèl kang unik banget. Potènsi hépatosit kanggo nglakokaké proliferasi, muncul nalika dumadi kélangan massa sèl,[22] kang diarani fasa prima utawa fasa kompetènsi réplikatif[23] kang lumrahé dipicu déning sèl Kupffer liwat sekresi sitokina IL-6 lan TNF-α. Ing fasa iki, hepatosit ngleboni siklus sèl saka fasa G0 menyang fasa G1.
TNF-α bisa mènèhaké èfèk proliferatif utawa apoptotik, gumantung ing spesi oksigèn réaktif lan glutathion, minimal 4 faktor transkripsi diaktivasi sadurungé hepatosit lumebu menyang njero fasa proliferasi, ya iku NF-κB, STAT-3, AP-1 lan C/EBP-beta.[24]
Proliferasi hépatosit diindhuksi déning stimulasi sitokina HGF lan TGF-α, lan EGF[24] kanthi rong lintasan. HGF, TGF-α, lan EGF wujud faktor patuwuhan kang asalé saka substrat serina lan protéin logam[25] kang ngindhuksi sintesis DNA.[23] Lintasan pisanan ya iku lintasan IL-6/STAT-3 kang duwé peran sajeroning siklus sèl liwat siklin D1/p21 lan pangreksan sèl kanthi paningkatan rasio FLIP, Bcl-2, Bcl-xL, Ref1, lan MnSOD. Lintasan kaloro ya iku lintasan PI3-K/PDK-1/Akt kang ngendhalèkaké ukuran sèl liwat molekul mTOR, saliyané minangka dat anti-apoptosis lan antioksidan.
Hormon tri-iodotironina, saliyané ngedhunaké kadhar kolesterol ing ati,[26] uga duwé kapasitas sajeroning proliferasi hépatosit minangka mitogen kang duwé peran ing siklin D1,[27] nambah rikat konsumsi O2 déning mitokondria kanthi ngaktivasi transkripsi ing gen ambegan nganti ngundhakaké prodhuksi spesi oksigèn réaktif.[28] Sekresi ROS menyang njero sitoplasma hépatosit bakal ngaktivasi faktor transkripsi NF-κB.[29] Ing sèl Kupffer, ROS sajeroning sitoplasma, bakal ngaktivasi sekresi sitokina TNF-α, IL-6 lan IL-1 kanggo disekresi. Ikatan kang dumadi antarané katelu sitokina iki karo hépatosit bakal ngindhuksi èksprèsi pancerep enzim antioksidan, kaya ta mangan superoksida dismutase, i-nitrogen monoksida sintase, protéin anti-apoptosis Bcl-2, haptoglobin lan fibrinogen-β kang diperlokaké hépatosit sajeroning proliferasi.[30] Stres oksidatif kang bisa ditimbulaké déning ROS uga karusakan kang bisa ditimbulaké déning manéka sitokina, bisa diilangaké kanthi asupan tosoferol (100 mg/kg) utawa senyawa panyandhet gadolinium klorida (10 mg/kg) kaya kang diduwèni déning sèl Kupffer, sadurungé stimulasi hormon tri-iodotironina,[31] éwadéné laju proliferasi hépatosit dikendhalèkaké déning kadhar etanolamina minangka faktor hepatotrofik humoral.[32]
Kamampuan ati kanggo ngèlakokaké régenerasi wis dikawruhi wiwit jaman Yunani kuna saka carita mitos ngenani sawijining titan kang jenengé Prometheus.[33] Kamampuan iki bisa sirna, nganti hépatosit ora bisa lumebu menyang njero siklus sèl, sanajan kèlangan sapérangan massané, yèn dumadi fibrosis ati. Lintasan fibrosis kang ora énggal éntuk parawatan, saya suwé bakal ngrembaka dadi sirosis ati[34] lan ngudokaké panandhangé kanggo nglakoni transplantasi ati utawa hépatèktomi kanggo tetep urip.
Régenerasi ati sawisé hépatèktomi parsial wujud prosès kang rumit banget ing sangisoré prabawa owah-owahan hémodinamika, modhulasi sitokina, hormon faktor patuwuhan lan aktivasi faktor transkripsi, kang ngarah ing prosès mitosis. Hormon PRL kang disekresi déning klanjer hipofisis ngindhuksi respon hépatotrofik minangka mitogen kang duwé peran sajeroning prosès proliferasi lan diferensiasi.[35] PRL mènèhi prabawa marang paningkatan aktivitas faktor transkripsi kang duwé peran sajeroning proliferasi sèl, kaya ta AP-1, c-Jun lan STAT-3; lan diferensiasi lan kareksané metabolisme, kaya ta C/EBP-alfa, HNF-1, HNF-4 lan HNF-3. c-Jun wujud salah siji protéin panyusun AP-1.[36] Indhuksi NF-κB ing fasa iki diperlokaké kanggo nyegah apoptosis lan micu derap siklus sèl kang wajar.[37] Ing wektu iki, peran retinil asetat dadi vital banget, amarga fungsiné kang nambah massa DNA lan protéin kang dikandhut.[38]
Lelara ing ati[besut | besut sumber]
Ati wujud organ kang nopang kalangsungan urip mèh kabèh organ liya ing njero awak. Amarga papan kang strategis banget lan fungsi multi-dimensional, ati dadi rentan banget marang tekané manéka lelara. Ati bakal ngrèspon manéka lelara mau kanthi ngradhang, kang diarani hepatitis
Asring uga hepatitis diwiwiti karo réaksi radhang patobiokimiawi kang diarani fibrosis hati,[39] kanthi simtoma paraklinis wujud paningkatan rasio plasma laminin, sawijining glikoprotein kang disekresi sèl Ito, asem hialuronat lan sajenis aminopeptida ya iku prokolagen jinis III,[40] dan CEA.[41] Fibrosis ati bisa disebabaké déning asoré rasio plasma HGF,[42][43] utawa amarga infèksi viral, kaya ta hepatitis B, patogen kang disebabaké déning infèksi akut sajenis virus DNA kang duwé fokus infèksi wujud cithakan transkripsi kang diarani cccDNA kang kametilasi,[44] utawa hepatitis C, patogen sarupa hepatitis B kang disebabaké déning infèksi virus RNA kanthi fokus infèksi wujud metilasi DNA, mligi liwat mékanisme èksprèsi genetik berkas GADD45B, saéngga ngakibataké siklus sèl hépatosit dadi kacandhet-candhet.[45][46]
Fibrosis ati merlokaké pananganan seawal mungkin, kaya ing modhèl tikus, stimulasi proliferasi hépatosit bakal ngluruhaké fokus infèksi virus hepatitis B,[47] sadurungé ngrembaka dadi sirosis ati utawa karsinoma hepatoselular. Sawisé dumadi kanker ati, senyawa siklosporina kang duwé potènsi kanggo micu proliferasi hépatosit, malah bakal nyepetaké ngrembakané sèl kanker,[48] amarga sèl kanker ngalami hiperplasia hépatik, ya iku proliferasi kang ora dibarengi aktivasi faktor transkripsi genetik. Iki bisa diindhuksi mawa stimulasi timbal nitrat (LN, 100 mikromol/kg), siproteron asetat (CPA, 60 mg/kg), lan nafenopin (NAF, 200 mg/kg).[49]
Hépatitis uga bisa diwiwiti kanthi defisiensi mitokondria ing njero hepatosit, kang diarani steatohepatitis. Disfungsi mitokondria bakal duwé dampak tumrap homeostasis senyawa lipid lan paningkatan rasio spesi oksigèn reaktif kang ngindhuksi TNF-α.[50] Iki bakal terus ing pangendhepan lemak, stres oksidatif lan peroksidasi lipid,[51] sarta marakaké mitokondria dadi rentan marang pepati déning nekrosis akibat asoré rasio ATP sajeroning matrik mitokondria, utawa déning apoptosis liwat pambentukan apoptosom lan paningkatan permeabilitas membran mitokondria kanthi mekanisme Fas/TNF-α. Panyuwunan ènergi kang dhuwur ing kaanan iki njalari mitokondria ora bisa mulihaké cadhangan ATP nganti bisa micu sirosis ati,[51] éwadéné peroksidasi lipid bakal njalari karusakan ing DNA mitokondria lan membran mitokondria sisih njero kang diarani sardiolipin, kanthi paningkatan laju oksidasi-beta asem lemak, bakal dumadi akumulasi èlèktron ing respiratory chain komplèks I lan III kang ngedhunaké kadhar antioksidan.[50]
Sèl hépatosit apoptotik bakal dicerna déning sèl Ito dadi fibrinogen kanthi réaksi fibrogenesis sawisé diaktivasi déning prodhuk saka peroksidasi lipid lan rasio leptin kang dhuwur. Apoptosis kronis banjur dikompènsasi kanthi paningkatan laju proliferasi hépatosit, dikanthèni DNA kang rusak déning disfungsi mitokondria, lan njalari mutasi genetik lan kanker.
Ing modhèl tikus, melatonin wujud senyawa kang ngedhunaké fibrosis ati,[52] sauntara ing modhèl klinci, kurkumin wujud senyawa organik kang ngedhunaké paraklinis steatohepatitis,[53] sauntara hormon serotonin[54] lan kurangé asupan metionina lan kolina[55] mènèhi èfèk suwaliké kanthi resistansi adiponektin.[56]
Disfungsi mitokondria uga tinemu ing kabèh patogenesis ati, saka kasus radhang nganti kanker lan transplantasi.[57] Ing kolestasis kronik, asem ursodeoksikolat bebarengan karo GSH silih sinergis minangka antioksidan kang ngreksa sardiolipin lan fosfatidil serina nganti nyegah dumadiné sirosis ati.[58]
Prabawa alkohol[besut | besut sumber]
Alkohol ditepungi duwé fungsi immunosupresif marang sistem kakebalan awak, kalebu ngredhem èksprèsi kluster diferensiasi CD4+ lan CD8+ kang diperlokaké sajeroning njaga tahaning ati marang infèksi viral, mligi HCV.[59] Alkohol uga ngredhem rasio kemokina IFN ing lintasan transduksi sinyal selular, saliyané ngundhakaké résiko dumadiné fibrosis.[60]
Akèh lintasan metabolisme mènèhi kontribusi marang alkohol kanggo ngindhuksi stres oksidatif.[61] Salah siji lintasan métabolisme kang asring diaktivasi déning etanol ya iku indhuksi enzim sitokrom P450 2E1. Enzim iki nimbulaké spesi oksigèn réaktif kaya radikal anion superoksida lan hidrogen peroksida, sarta ngaktivasi subtrat toksik kalebu etanol dadi prodhuk kang luwih réaktif lan toksik. Sèl dendritik katoné wujud sèl kang paling kaprabawa déning kandhutan etanol ing njero alkohol. Ing pacobèn migunakaké modhèl tikus, etanol ngundhakaké rasio plasma IL-1β, IL-6, IL-8, TNF-α, AST, ALT, ADH, γ-GT, TG, MDA lan ngredham rasio IL-10, GSH,[62] faktor transkripsi NF-κB lan AP-1.[63]
Prabawa alkaloid[besut | besut sumber]
Kopi, salah siji komplèks senyawa alkaloid saka golongan purina xantina karo asem klorogenat lan lignan,[64] ing studi epidemiologis, disimpulaké minangka salah siji faktor pamudhun risiko dumadiné diabetes mellitus jinis 2,[65][66] lelara Parkinson, sirosis ati lan karsinoma hepatoselular,[67] lan saya apiké toleransi glukosa.[64] Konsumsi kopi kanthi kronis kabukti ora njalari tekanan getih dhuwur nanging kanthi akut ngakibataké paningkatan tekanan getih sauntara sajeroning selang wektu cendhak,[68] lan plasma homosisteina[67] saéngga bisa dadi ancaman kanggo panandhang gangguan kardiovaskular.[65]
Konsumsi kopi kanthi teratur bisa ngedhunaké rasio enzim ALT sarta aktivitas enzimatik ing lintasan métabolisme ati,[69] kang asring disebabaké déning[70] infèksi viral, indhuksi usada, karacunan, kaanan iskemik, steatosis (akibat alkohol, diabetes, obesitas), lelara otoimun,[71] lan resistansi insulin, sindrom metabolisme,[72] lan kakèhen dat wesi.[73] Saliyané ALT, kopi uga ngedhunaké enzim ati liyané, ya iku gamma-GT lan alkalina fosfatase.[74] lan mènèhi èfèk antioksidan lan detoksifikasi fasa II amarga senyawa diterpena, kafestol lan kahweol,[75] saéngga nyegah dumadiné prosès karsinogenesis.[76][77] Prosès tersebut dibarengi dengan gamma-GT sebagai indikator utama.[78]
Transplantasi ati[besut | besut sumber]
Tèknologi transplantasi ati wujud asil kang dikembangaké saka panlitèn ing sapérangan babagan studi kadhokteran. Ing taun 1953, Billingham, Brent, lan Medawar nemu yèn toléransi kimerisme[79] bisa diindhuksi déning infus sèl hematolimfopoietik donor ing modhèl tikus.[80]
Nalika taun 1958 studi canine ngembangaké sawijining téyori ngenani molekul hépatotrofik ing portal pambuluh walik ing ati lan nemu hormon insulin minangka faktor hépatotrofik utama saka sapérangan faktor liya kang ana.[81] Ing wektu kang mèh bebarengan téyori ngenani transplantasi multiviseral lan ati uga ngrembaka saka studi imunosupresi kang nyinaoni algoritma empiris saka pangenalan pola lan rèspon térapis. Nalika awal 1960, dibuktèkaké yèn canine lan allograft manungsa nduwé toléransi kimersime kang bisa kaindhuksi otomatis kanthi bantuan imunosupresi, nganti akir 1962 disimpulaké kanthi klèru, yèn transplantasi nglibataké loro sistem kakebalan kang béda. Konsekwènsi kasimpulan mau dadi dogma yèn tolerogenisitas ati, dhasaré béda, ora mung karo sungsum balung mburi, nanging karo kabèh organ awak liyané.[80] Keklèron iki ora kakorèksi kanthi becik tekan taun 1990.[79]
Transplantasi ati kang pisanan dilakokaké ing Denver nalika taun 1963,[82] pisanan kasil kacathet nalika taun 1967 kanthi azatioprina, prednison lan globulin anti-limfoid, déning Thomas E. Starzl saka Amérikah Sarékat, disusul déning kasilé transplantasi sungsum balung mburi manungsa nalika taun 1968.[79] Rentang wektu antara taun 1967 tekan 1979 nyathet kaping 84 transplantasi ati ing bocah kanthi 30% daya tahan urip tekan 2 taun.[82]
Nrembakané studi imunosupresi banjur mènèhaké kabecikan lan pangarep-arep urip luwih dawa kanggo pasien, antarané kanthi panggantian azatioprina mawa siklosporina nalika taun 1979, banjur kagantèkaké mawa takrolimus nalika taun 1989.[81]
Nalika taun 1992, dikembangaké téyori mikrokimerisme leukosit donor[83] kanthi cakupan donor saka silsilah kang béda, kang mènèhaké pangarep-arep urip kang dawa banget kanggo panampa donor organ, sawisé dikawruhi gegandhèngan antarané aspèk imunologis saka transplantasi, infèksi, toléransi déning sungsum balung mburi, neoplasma lan kelainan otoimun, kang diarani mekanisme seminal. Rèspon kakebalan lan toléransi kakebalan antarané organ donor lan awak tinemu wujud fungsi saka migrasi lan lokalisasi leukosit.[80] Salah siji temuané ya iku aktivasi sistem kakebalan turunan déning sèl NK lan interferon-γ langsung sawisé transplantasi rampung dilakokaké.[84] Ing modhèl tikus, sèl hépatosit donor tinemu asifat antigenik banget saéngga njalari rèspon panulakan, kang bisa dilakokaké kanthi swatantra utawa bebarengan antarané sèl T CD4 lan sèl T CD8.[85]
Kanggo iku diperlokaké terapi imunosupresif kang intensif sadurungé transplantasi dilakokaké, kang diarani preparative regimen utawa conditioning kanggo nyegah panulakan organ donor déning sistem kakebalan inang.[86] Terapi imunosupresif mau ditujokaké kanggo nekan sèl T lan sèl NK inang guna mènèhaké ruwang ing njero sungsum balung mburi kanggo transplantasi sèl punca hematopoietik saka organ donor liwat terapi mielosupresif, kanggo kaseimbangan répopulasi sèl donor karo sèl asil diferensiasi saka sèl punca inang.
Diwasa iki, transplantasi ati dilakokaké mung nalika ati wis lumebu jenjang akir sawijining lelara, utawa wis dadi disfungsi akut kang diarani fulminant hepatic failure. Kasus transplantasi ati ing manungsa lumrahé disebabaké déning sirosis ati akibat saka hépatitis C kronis, katergantungan alkohol, hepatitis otoimun lsp.
Tèknik umum kang dipigunakaké ya iku transplantasi ortotopik, ya iku panempatan organ donor ing posisi anatomik kang padha karo posisi awal organ sadurungé. Transplantasi ati duwé potènsi bisa ditrepaké, mung yèn panampa organ donor ora duwé kaanan liya kang ngeboti, kaya ta kanker metastatis ing njaba organ ati, katergantungan marang usada utawa alkohol. Sapérangan ahli duwé pedoman ing kriteria Milan kanggo selèksi pasien transplantasi ati.
Organ donor, diarani allograft, lumrahé asalé saka manungsa liya kang nembé nilar donya akibat tatu utek traumatik (kadaverik). Tèknik transplantasi liya migunakaké organ manungsa kang isih urip, oprasi hepatektomi ngangkat 20% ati ing sègmèn Coinaud 2 lan 3 saka wong diwasa kanggo didonoraké marang sawijining bocah, nalika taun 1989.
Wacan terusan[besut | besut sumber]
- [1] Èksprèsi genetik kang diindhuksi déning hormon tri-iodotironina lan GH
Rujukan[besut | besut sumber]
- ↑ Physiology at MCG 6/6ch2/s6ch2_30
- ↑ "Cooperation of liver cells in health and disease". Medical University of Gdansk, Department of Histology and Immunology; Kmieć Z. Dibukak ing 2010-07-30.
- ↑ "An experimental analysis of liver development". Douarin NM. Dibukak ing 2010-10-11.
- ↑ "Hepatocyte differentiation initiates during endodermal-mesenchymal interactions prior to liver formation". Section of Biochemistry, Brown University; Cascio S, Zaret KS. Dibukak ing 2010-10-11.
- ↑ a b "The role of hepatocytes and oval cells in liver regeneration and repopulation". Department of Pathology, University of Washington; Fausto N, Campbell JS. Dibukak ing 2010-08-01.
- ↑ "Ductular hepatocytes". Medical College of Virginia, Virginia Commonwealth University; Sirica AE. Dibukak ing 2010-08-01.
- ↑ "Stem cells, cell transplantation and liver repopulation". Marion Bessin Liver Research Center, Division of Hepatology, Department of Medicine, Albert Einstein College of Medicine of Yeshiva University; Oertel M, Shafritz DA. Dibukak ing 2010-08-01.
- ↑ "Hepatic progenitor cells, stem cells, and AFP expression in models of liver injury". Division of Radiooncology, Deutsches Krebsforschungszentrum; Kuhlmann WD, Peschke P. Dibukak ing 2010-08-01.
- ↑ "Hepatic stem cells: a review". Department of Anatomical Pathology, University of Cape Town; Vessey CJ, de la Hall PM. Dibukak ing 2010-08-01.
- ↑ "Epimorphin regulates bile duct formation via effects on mitosis orientation in rat liver epithelial stem-like cells". Stem Cell and Regenerative Medicine Lab, Beijing Institute of Transfusion Medicine; Zhou J, Zhao L, Qin L, Wang J, Jia Y, Yao H, Sang C, Hu Q, Shi S, Nan X, Yue W, Zhuang F, Yang C, Wang Y, Pei X. Dibukak ing 2010-10-11.
- ↑ "Ductular hepatocytes". Medical College of Virginia, Virginia Commonwealth University; Sirica AE. Dibukak ing 2010-08-01.
- ↑ "Bone marrow-derived hepatic oval cells differentiate into hepatocytes in 2-acetylaminofluorene/partial hepatectomy-induced liver regeneration". Department of Pathology, Immunology and Laboratory Medicine, University of Florida College of Medicine,; Oh SH, Witek RP, Bae SH, Zheng D, Jung Y, Piscaglia AC, Petersen BE. Dibukak ing 2010-08-01.
- ↑ "Bone marrow as a potential source of hepatic oval cells". Department of Pathology, School of Medicine, University of Pittsburgh; Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan AK, Murase N, Boggs SS, Greenberger JS, Goff JP. Dibukak ing 2010-08-01.
- ↑ "Granulocyte-colony stimulating factor promotes liver repair and induces oval cell migration and proliferation in rats". Department of Pathology, Immunology and Laboratory Medicine, College of Medicine, University of Florida; Piscaglia AC, Shupe TD, Oh SH, Gasbarrini A, Petersen BE. Dibukak ing 2010-08-01.
- ↑ "Activation, proliferation, and differentiation of progenitor cells into hepatocytes in the D-galactosamine modhèl of liver regeneration". Marion Bessin Liver Research Center, Albert Einstein College of Medicine; Dabeva MD, Shafritz DA. Dibukak ing 2010-08-01.
- ↑ "The effect of prednisolone and a protéin-deficient diet on plasma albumin and fibrinogen in a turpentine-induced acute-phase reaction in rats". Department of Internal Medicine, University of Berne; Ballmer PE, Studer H. Dibukak ing 2010-08-02.
- ↑ "Hepatic Stellate Cell in Fibrosis: Stellate Cell Activation". Division of Liver Diseases, Mount Sinai School of Medicine; Scott L. Friedman. Dibukak ing 2010-10-16.
- ↑ "Insulin Action in Hyperthyroidism: A Focus on Muscle and Adipose Tissue". Hellenic National Center for Research, Prevention, and Treatment of Diabetes Mellitus and Its Complications, et al; Mitrou P, Raptis SA, Dimitriadis G. Dibukak ing 2010-08-07.
- ↑ "Glucagon deficiency reduces hepatic glucose production and improves glucose tolerance in adult mice". Department of Pathology and Laboratory Medicine, Children's Hospital of Philadelphia; Hancock AS, Du A, Liu J, Miller M, May CL. Dibukak ing 2010-08-07.
- ↑ "Hypothalamic integration of portal glucose signals and control of food intake and insulin sensitivity". Inserm U855, Institut national de la santé et de la recherche médicale, faculté de médecine Laennec; Delaere F, Magnan C, Mithieux G. Dibukak ing 2010-08-07.
- ↑ "Molecular mechanisms of liver regeneration and protection for treatment of liver dysfunction and diseases". Department of General Surgery, Hokkaido University School of Medicine; Fujiyoshi M, Ozaki M. Dibukak ing 2010-07-30.
- ↑ "The role of cytokines in liver failure and regeneration: potential new molecular therapies". The Goldyne Savad Institute for Gene Therapy, Hadassah Hebrew University Hospital,; Galun E, Axelrod JH. Dibukak ing 2010-07-30.
- ↑ a b "Liver regeneration. 2. Role of growth factors and cytokines in hepatic regeneration". Department of Pathology and Laboratory Medicine, Brown University,; Fausto N, Laird AD, Webber EM. Dibukak ing 2010-07-30.
- ↑ a b "Liver regeneration". Department of Pathology, University of Washington School of Medicine; Fausto N. Dibukak ing 2010-07-30.
- ↑ "A molecular view of liver regeneration". Department of Pathology, FMRP, USP, Brazil.; Tarlá MR, Ramalho FS, Ramalho LN, Silva Tde C, Brandão DF, Ferreira J, Silva Ode C, Zucoloto S. Dibukak ing 2010-07-30.
- ↑ "Regulation of thyroid hormone activation via the liver X-receptor/retinoid X-receptor pathway". Human and Natural Sciences Center, Federal University of ABC; Christoffolete MA, Doleschall M, Egri P, Liposits Z, Zavacki AM, Bianco AC, Gereben B. Dibukak ing 2010-08-01.
- ↑ "Triiodothyronine stimulates hepatocyte proliferation in two models of impaired liver regeneration". Department of Toxicology, Oncology and Molecular Pathology Unit, University of Cagliari,; Columbano A, Simbula M, Pibiri M, Perra A, Deidda M, Locker J, Pisanu A, Uccheddu A, Ledda-Columbano GM. Dibukak ing 2010-08-01.
- ↑ "Hormetic responses of thyroid hormone calorigenesis in the liver: Association with oxidative stress". Molecular and Clinical Pharmacology Program, Institute of Biomedical Sciences, Faculty of Medicine, University of Chile; Videla LA. Dibukak ing 2010-08-19.
- ↑ "Thyroid hormone-induced oxidative stress triggers nuclear factor-kappaB activation and cytokine gene expression in rat liver". Programa de Farmacologíca Molecular y Clínica, Instituto de Ciencias Biomédicas, Universidad de Chile; Tapia G, Fernández V, Varela P, Cornejo P, Guerrero J, Videla LA. Dibukak ing 2010-08-01.
- ↑ "Hormetic responses of thyroid hormone calorigenesis in the liver: Association with oxidative stress". Molecular and Clinical Pharmacology Program, Institute of Biomedical Sciences, Faculty of Medicine, University of Chile; Videla LA. Dibukak ing 2010-08-01.
- ↑ "Redox regulation of thyroid hormone-induced Kupffer cell-dependent IkappaB-alpha phosphorylation in relation to inducible nitric oxide synthase expression". Molecular and Clinical Pharmacology Program, Institute of Biomedical Sciences, Faculty of Medicine, University of Chile; Fernández V, Tapia G, Varela P, Videla LA. Dibukak ing 2010-08-01.
- ↑ "Ethanolamine modulates the rate of rat hepatocyte proliferation in vitro and in vivo". Meiji Institute of Health Sciences; Sasaki H, Kume H, Nemoto A, Narisawa S, Takahashi N. Dibukak ing 2010-08-01.
- ↑ "The myth of Prometheus and the liver". Department of Pathology, East Orange Veterans Affairs Medical Center; T S Chen dan P S Chen. Dibukak ing 2010-08-01.
- ↑ "Reversal of liver fibrosis". Department of Internal Medicine, Division of Gastroenterology at King Fahad Hospital of the University; Ismail MH, Pinzani M. Dibukak ing 2010-08-01.
- ↑ "Prolactin's role in the early stages of liver regeneration in rats". Departamento de Biología Molecular, Facultad de Ciencias C-V, Universidad Autónoma de Madrid; Olazabal IM, Muñoz JA, Rodríguez-Navas C, Alvarez L, Delgado-Baeza E, García-Ruiz JP. Dibukak ing 2010-08-04.
- ↑ "Signal transduction during liver regeneration". Department of Medicine, University of North Carolina at Chapel Hill; Brenner DA. Dibukak ing 2010-08-04.
- ↑ "NFkappaB prevents apoptosis and liver dysfunction during liver regeneration". Department of Medicine, The University of North Carolina at Chapel Hill,; Iimuro Y, Nishiura T, Hellerbrand C, Behrns KE, Schoonhoven R, Grisham JW, Brenner DA. Dibukak ing 2010-08-04.
- ↑ "Effect of Depletion of Vitamin A, followed by Supplementation with Retinyl Acetate or Retinoic Acid, on Regeneration of Rat Liver" (PDF). Department of Biochemistry, Indian Institute of Science; M. JAYARAM, K. SARADA dan J. GANGULY. Dibukak ing 2010-12-08.
Although the rates of increase in the DNA and protéin contents reflected the rates of regeneration in all the groups, the RNA values followed a rather different pattern, in that they showed a striking increase immediately after supplementation with retinyl acetate (after the surgery),
- ↑ "Non-invasive assessment of liver fibrosis in chronic liver diseases: Implementation in clinical practice and decisional algorithms". Department of Digestive Diseases, Hepatology and Clinical Nutrition, Dell’Angelo Hospital; Giada Sebastiani. Dibukak ing 2010-10-09.
Formation and accumulation of fibrosis in the liver is the common pathway that leads to an evolutive liver disease
- ↑ "Biochemical markers of hepatic fibrosis". Department of Clinical Biochemistry, University of Padova; Plebani M, Burlina A. Dibukak ing 2010-08-02.
- ↑ "Evaluation of the behavior of carcinoembryonic antigen in cirrhotic patients". Service of Internal Medicine, Hospital de Galdacano; Collazos J, Genollà J, Ruibal A. Dibukak ing 2010-08-02.
- ↑ "Hepatocyte growth factor: a regenerative drug for acute hepatitis and liver cirrhosis". Division of Molecular Regenerative Medicine, Department of Biochemistry and Molecular Biology, Osaka University Graduate School of Medicine; Mizuno S, Nakamura T. Dibukak ing 2010-07-28.
- ↑ "Growth inhibition and apoptosis in liver myofibroblasts promoted by hepatocyte growth factor leads to resolution from liver cirrhosis". Division of Molecular Regenerative Medicine, Course of Advanced Medicine, Osaka University Graduate School of Medicine; Kim WH, Matsumoto K, Bessho K, Nakamura T. Dibukak ing 2010-07-28.
- ↑ "Evidence that methylation of hepatitis B virus covalently closed circular DNA in liver tissues of patients with chronic hepatitis B modulates HBV replication". State Key Laboratory of Cancer Biology, Department of Pharmacogenomics, School of Pharmacy, The Fourth Military Medical University; Guo Y, Li Y, Mu S, Zhang J, Yan Z. Dibukak ing 2010-08-02.
- ↑ "Downregulation of Gadd45beta expression by hepatitis C virus leads to defective cell cycle arrest". Institut National de la Santé et de la Recherche Médicale U955; Higgs MR, Lerat H, Pawlotsky JM. Dibukak ing 2010-08-02.
- ↑ "Hypermethylation of growth arrest DNA damage-inducible gene 45 beta promoter in human hepatocellular carcinoma". Department of Medical Oncology and Therapeutic Research, City of Hope National Medical Center; Qiu W, Zhou B, Zou H, Liu X, Chu PG, Lopez R, Shih J, Chung C, Yèn Y. Dibukak ing 2010-08-02.
- ↑ "In vivo proliferation of hepadnavirus-infected hepatocytes induces loss of covalently closed circular DNA in mice". Department of Medicine, University Medical Center Hamburg-Eppendorf,; Lutgehetmann M, Volz T, Köpke A, Broja T, Tigges E, Lohse AW, Fuchs E, Murray JM, Petersen J, Dandri M. Dibukak ing 2010-08-02.
- ↑ "Cyclosporine stimulates hepatocyte proliferation and accelerates development of hepatocellular carcinomas in rats". Department of Pathology, University of Pittsburgh School of Medicine,; Masuhara M, Ogasawara H, Katyal SL, Nakamura T, Shinozuka H. Dibukak ing 2010-08-01.
- ↑ "Liver cell proliferation induced by nafenopin and cyproterone acetate is not associated with increases in activation of transcription factors NF-kappaB and AP-1 or with expression of tumor necrosis factor alpha". Dipartimento di Biochimica, Università di Verona; Menegazzi M, Carcereri-De Prati A, Suzuki H, Shinozuka H, Pibiri M, Piga R, Columbano A, Ledda-Columbano GM. Dibukak ing 2010-08-01.
- ↑ a b "Mitochondrial injury in steatohepatitis". Institut National de la Santé et de la Recherche Médicale (INSERM) Unité 481, Faculté de Médecine Xavier Bichat; Pessayre D, Fromenty B, Mansouri A. Dibukak ing 2010-08-05.
- ↑ a b "Mitochondrial involvement in non-alcoholic steatohepatitis". Department of Medical and Occupational Sciences, University of Foggia; Serviddio G, Sastre J, Bellanti F, Viña J, Vendemiale G, Altomare E. Dibukak ing 2010-08-05.
- ↑ "Melatonin ameliorates experimental hepatic fibrosis induced by carbon tetrachloride in rats". Department of Geriatrics Medicine, The First Affiliated Hospital of Anhui Medical University; Hong RT, Xu JM, Mèi Q. Dibukak ing 2010-08-05.
- ↑ "Curcumin ameliorates rabbits's steatohepatitis via respiratory chain, oxidative stress, and TNF-alpha". Department of Biochemistry and Molecular Biology II, 18071 University of Granada; Ramirez-Tortosa MC, Ramirez-Tortosa CL, Mesa MD, Granados S, Gil A, Quiles JL. Dibukak ing 2010-08-05.
- ↑ "Serotonin mediates oxidative stress and mitochondrial toxicity in a murine modhèl of nonalcoholic steatohepatitis". Switserlan Hepato-Pancreato-Biliary Center, Department of Visceral and Transplantation Surgery, University Hospital Zurich; Nocito A, Dahm F, Jochum W, Jang JH, Georgiev P, Bader M, Renner EL, Clavien PA. Dibukak ing 2010-08-05.
- ↑ "Pentoxifylline attenuates steatohepatitis induced by the methionine choline deficient diet". Department of Medicine, Division of Hepatology, Feinberg School of Medicine, Northwestern University; Koppe SW, Sahai A, Malladi P, Whitington PF, Green RM. Dibukak ing 2010-08-05.
- ↑ "MCD-induced steatohepatitis is associated with hepatic adiponectin resistance and adipogenic transformation of hepatocytes". ANU Medical School, Ostralin National University at The Canberra Hospital,; Larter CZ, Yeh MM, Williams J, Bell-Anderson KS, Farrell GC. Dibukak ing 2010-08-05.
- ↑ "Targeting Mitochondria: A New Promising Approach for the Treatment of Liver Diseases". Centre for the Study of Liver Diseases, Department of Medical and Occupational Sciences; Serviddio G, Bellanti F, Sastre J, Vendemiale G, Altomare E. Dibukak ing 2010-08-05.
- ↑ "Ursodeoxycholic acid protects against secondary biliary cirrhosis in rats by preventing mitochondrial oxidative stress". Department of Medical and Occupational Sciences, University of Foggia; Serviddio G, Pereda J, Pallardó FV, Carretero J, Borras C, Cutrin J, Vendemiale G, Poli G, Viña J, Sastre J. Dibukak ing 2010-08-05.
- ↑ "Hepatitis C Virus and Alcohol". Warren Alpert Medical School of Brown University; Larry Siu, Julie Foont, dan Jack R. Wands. Dibukak ing 2010-10-09.
- ↑ "Hazardous drinking is associated with elevated aspartate aminotransferase to platelet ratio index in an urban HIV clinical cohort". Department of Medicine, Johns Hopkins University School of Medicine, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health; Amina A. Chaudhry, Mark S. Sulkowski, Geetanjali Chander, dan Richard D. Moore. Dibukak ing 2010-10-09.
- ↑ "CYP2E1 and Oxidative Liver Injury by Alcohol". Department of Pharmacology and Systems Therapeutics, Mount Sinai School of Medicine; Yongke Lu dan Arthur I. Cederbaum. Dibukak ing 2010-10-13.
- ↑ "Protective effects of quercetin on liver injury induced by ethanol". Institute of Medicinal Plant Development, Chinese Academy of Medical Sciences, Peking Union Medical College; Xi Chen. Dibukak ing 2010-10-11.
- ↑ "Ethanol prevents development of destructive arthritis". Department of Rheumatology and Inflammation Research, Center for Bone Research at the Sahlgrenska Academy, Göteborg University, Section for Medical Inflammation Research, Lund University; Ing-Marie Jonsson, Margareta Verdrengh, Mikael Brisslert, Sofia Lindblad, Maria Bokarewa, Ulrika Islander, Hans Carlsten, Claes Ohlsson, Kutty Selva Nandakumar, Rikard Holmdahl, dan Andrej Tarkowski. Dibukak ing 2010-10-11.
- ↑ a b "Coffee and type 2 diabetes: from beans to beta-cells". Department of Nutrition, Harvard School of Public Health; van Dam RM. Dibukak ing 2010-10-12.
- ↑ a b "Coffee, diabetes, and weight control". Department of Health and Nutrition Sciences, Brooklyn College, City University of New York; Greenberg JA, Boozer CN, Geliebter A. Dibukak ing 2010-10-12.
- ↑ "Coffee consumption and risk for type 2 diabetes mellitus". Harvard School of Public Health, Channing Laboratory, Harvard Medical School, and Brigham and Women's Hospital; Salazar-Martinez E, Willett WC, Ascherio A, Manson JE, Leitzmann MF, Stampfer MJ, Hu FB. Dibukak ing 2010-10-12.
- ↑ a b "Coffee and health: a review of recent human research". Linus Pauling Institute, Oregon State University; Higdon JV, Frei B. Dibukak ing 2010-10-12.
- ↑ "Coffee and coronary heart disease: a review". Department of Medicine, University of Tennessee; Rosmarin PC. Dibukak ing 2010-10-12.
- ↑ "Coffee: good, bad, or just fun? A critical review of coffee's effects on liver enzymes". Division of Gastroenterology, Hepatology, and Nutrition, Loyola University Medical Center; Homan DJ, Mobarhan S. Dibukak ing 2010-10-13.
- ↑ "[Increase of aminotransferases]". Clinique médicale, CHU de Rouen; Trivalle C, Chassagne P, Doucet J, Perol MB, Landrin I, Manchon ND, Bourreille J, Bercoff E. Dibukak ing 2010-10-13.
- ↑ "[Interpretation of hypertransaminasemia]". Service de médecine interne Hôpital Principal d'Instruction de Tunis; Othmani S, Bahri M, Bahri M. Dibukak ing 2010-10-13.
- ↑ "Contribution of metabolic factors to alanine aminotransferase activity in persons with other causes of liver disease". Gastroenterology, Metabolism, Endocrinology and Nutrition, Department of Medicine, Veterans Affairs Puget Sound Health Care System; Ioannou GN, Weiss NS, Boyko EJ, Kahn SE, Lee SP. Dibukak ing 2010-10-13.
- ↑ "Coffee and caffeine consumption reduce the risk of elevated serum alanine aminotransferase activity in the United States". Social & Scientific Systems Inc.,; Ruhl CE, Everhart JE. Dibukak ing 2010-10-13.
- ↑ "Unexpected effects of coffee consumption on liver enzymes". Istituto di Medicina Clinica, Università di Padova; Casiglia E, Spolaore P, Ginocchio G, Ambrosio GB. Dibukak ing 2010-10-13.
- ↑ "Induction of cancer chemopreventive enzymes by coffee is mediated by transcription factor Nrf2. Evidence that the coffee-specific diterpenes cafestol and kahweol confer protection against acrolein". Biomedical Research Centre, Ninewells Hospital and Medical School, University of Dundee; Higgins LG, Cavin C, Itoh K, Yamamoto M, Hayes JD. Dibukak ing 2010-10-13.
- ↑ "The multifaceted mechanisms for coffee's anti-tumorigenic effect on liver". Department of Hepatobiliary Surgery, Xijing Hospital, Fourth Military Medical University; Tao KS, Wang W, Wang L, Cao DY, Li YQ, Wu SX, Dou KF. Dibukak ing 2010-10-13.
- ↑ "Influence of coffee drinking on subsequent risk of hepatocellular carcinoma: a prospective study in Japan". Epidemiology and Prevention Division, Research Center for Cancer Prevention and Screening, National Cancer Center; Inoue M, Yoshimi I, Sobue T, Tsugane S; JPHC Study Group. Dibukak ing 2010-10-13.
- ↑ "Joint effects of coffee consumption and serum gamma-glutamyltransferase on the risk of liver cancer". Department of Public Health, University of Helsinki; Hu G, Tuomilehto J, Pukkala E, Hakulinen T, Antikainen R, Vartiainen E, Jousilahti P. Dibukak ing 2010-10-13.
- ↑ a b c "History of clinical transplantation". Thomas E. Starzl Transplantation Institute, University of Pittsburgh Medical Center,; Starzl TE. Dibukak ing 2010-08-04.
- ↑ a b c "The mystique of hepatic tolerogenicity". Transplantation Institute, Departments of Surgery, Pathology, and Pediatrics, University of Pittsburgh Medical Center; Starzl TE, Murase N, Demetris A, Trucco M, Fung J. Dibukak ing 2010-08-04.
- ↑ a b "History of clinical transplantation". Thomas E. Starzl Transplantation Institute, University of Pittsburgh; Starzl TE. Dibukak ing 2010-08-04.
- ↑ a b "History of pediatric liver transplantation. Where are we coming from? Where do we stand?". Department of Pediatric Surgery and Liver Transplantation, Université Catholique de Louvain; Otte JB. Dibukak ing 2010-08-04.
- ↑ "The unfinished legacy of liver transplantation: emphasis on immunology". Transplantation Institute, Department of Surgery, University of Pittsburgh Medical Center; Starzl TE, Lakkis FG. Dibukak ing 2010-08-04.
- ↑ "Activation of innate immunity (NK/IFN-gamma) in rat allogeneic liver transplantation: contribution to liver injury and suppression of hepatocyte proliferation". Department of Hepatobiliary Surgery, First Affiliated Hospital, Zhejiang University School of Medicine; Shen K, Zheng SS, Park O, Wang H, Sun Z, Gao B. Dibukak ing 2010-08-04.
- ↑ "Unusual patterns of alloimmunity evoked by allogeneic liver parenchymal cells". The Ohio State University College of Medicine, Department of Surgery; Bumgardner GL, Orosz CG. Dibukak ing 2010-08-04.
- ↑ Kufe, Donald W.; Pollock, Raphael E.; Weichselbaum, Ralph R.; Bast, Robert C., Jr.; Gansler, Ted S.; Holland, James F.; Frei III, Emil. (2003). Holland-Frei Cancer medicine. Dana-Farber Cancer Institute, Harvard Medical School Boston, Department of Surgical Oncology, University of Texas, MD Anderson Cancer Center, Department of Radiation and Cellular Oncology, University of Chicago Hospital, Chicago Tumor Institute, University of Chicago Chicago, University of Texas, MD Anderson Cancer Center, Houston, American Cancer Society, Derald H Ruttenberg Cancer Center, Mount Sinai School of Medicine New York (édhisi ka-6). Hamilton on BC Decker Inc.,. kc. Engraftment of Allogeneic Hematopoietic Transplants. ISBN 1-55009-213-8. Dibukak ing 2010-08-09.
{{cite book}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link)
Pranala njaba[besut | besut sumber]
| Wikimedia Commons duwé médhia ngenani Category:Liver. |
